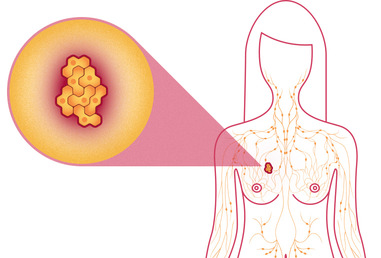
Theragenomic Medicine: Palbociclib (Ibrance) approved for postmenopausal women with advanced (metastatic) breast cancer
Last Updated on February 8, 2015 by Joseph Gut – thasso
Ibrance works by inhibiting molecules, known as cyclin-dependent kinases (CDKs) 4 and 6, involved in promoting the growth of cancer cells. Ibrance is intended for postmenopausal women with estrogen receptor (ER)-positive, human epidermal growth factor receptor 2 (HER2)-negative metastatic breast cancer who have not yet received an endocrine-based therapy. It is to be used in combination with letrozole, another FDA-approved product used to treat certain kinds of breast cancer in postmenopausal women and provides a novel treatment option to women diagnosed with metastatic breast cancer, according to Richard Pazdur, M.D., director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
The drug’s efficacy was demonstrated in 165 postmenopausal women with ER-positive, HER2-negative advanced breast cancer who had not received previous treatment for advanced disease. Clinical study participants were randomly assigned to receive Ibrance in combination with Letrozole (Femara) or Letrozole alone. Participants treated with Ibrance plus letrozole lived about 20.2 months without their disease progressing (progression-free survival), compared to about 10.2 months seen in participants receiving only letrozole. Information on overall survival is not available at this time.
The most common side effects of the drug were a decrease in infection-fighting white blood cells called neutrophils (neutropenia), low levels of white blood cells (leukopenia), fatigue, low red blood cell counts (anemia), upper respiratory infection, nausea, inflammation of the lining of the mouth (stomatitis), hair loss (alopecia), diarrhea, low blood platelet counts (thrombocytopenia), decreased appetite, vomiting, lack of energy and strength (asthenia), damage to the peripheral nerves (peripheral neuropathy) and nosebleed (epistaxis). Healthcare professionals should inform patients of these risks. It is recommended that treatment begin with a 125 milligram dose for 21 days, followed by seven days without treatment. Healthcare professionals are advised to monitor complete blood count prior to start of therapy and at the beginning of each cycle, as well as on Day 14 of the first two cycles, and as clinically indicated.

