Do genes affect our risk for addiction?

Last Updated on November 10, 2022 by Joseph Gut – thasso
November 10, 2022 – Drug addiction is a huge social problem of our todays societies. The problem does not only exist in the USA, but in other countries worldwide as well, with enormous numbers of victims due to alcoholism, smoking, and opioid and illicit drug use. Addiction and its associated habits, however, may change over time, based on societal, economical, and medical changements and developments.
 Every person responds to drugs and medications differently. Maybe you’ve even experienced it. Say you take a medication and it works well. But the same pill does nothing for one friend and makes another feel sick. The same is true for the behaviour in the face of alcohol, or opioids, or illicit drugs. Some individuals take them once, and never develop an urge to take them again and again. Other individuals cannot withstand it and have to take them again and again, even tough often they do not even willingly want to do so. People get caught in addiction.
Every person responds to drugs and medications differently. Maybe you’ve even experienced it. Say you take a medication and it works well. But the same pill does nothing for one friend and makes another feel sick. The same is true for the behaviour in the face of alcohol, or opioids, or illicit drugs. Some individuals take them once, and never develop an urge to take them again and again. Other individuals cannot withstand it and have to take them again and again, even tough often they do not even willingly want to do so. People get caught in addiction.
As in the cases of differences in responses of individual patients to therapeutic drugs, or the tendency of developing adverse drug responses (ADR’s), differences like these are often caused by differences in genes. Thus, in the field of addiction, scientists started to look for “addiction genes,” in order to help to explain biological differences that may make a person more or less vulnerable to addiction. Such addiction-related genes, or more precisely genetic variations thereof may be associated with responses such as a vulnerable person may have a high preference for a particular substance, or experience extreme withdrawal symptoms if they try to quit. On the other hand, a person may be less vulnerable if they feel no pleasure from a drug that makes others euphoric.
Of course, no one is born destined to develop substance use disorder. Like in most other diseases, the person’s genes, the person’s environment , and possibly many other confounding factors together determine the risk for addiction. Just because you (genetically) are prone to addiction doesn’t mean you’re going to become addicted. It may just mean that you’ve got to be careful.
Addiction Runs in Families
What are the hints that developing addiction has a genetic basis? For one, substance use disorder often runs in families. The figure to the left illustrates this observation by means of a pedigree (family 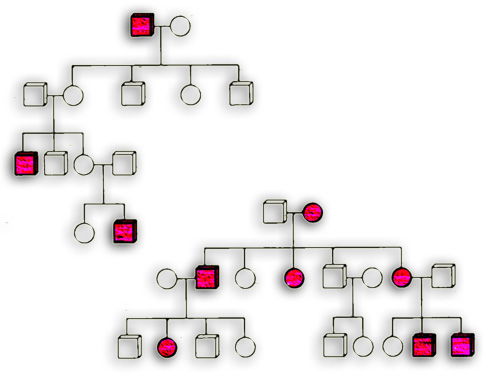 tree) showing show affected people in red and unaffected family members in white. This points to an inherited component, meaning it can pass from parent to child by way of genes. For this reason, family histories offer clues about how vulnerable to addiction you as an individual might be. For example, if you have a close relative that’s affected, it’s a clue to be extra careful.
tree) showing show affected people in red and unaffected family members in white. This points to an inherited component, meaning it can pass from parent to child by way of genes. For this reason, family histories offer clues about how vulnerable to addiction you as an individual might be. For example, if you have a close relative that’s affected, it’s a clue to be extra careful.
Researchers use family histories too. They compare DNA sequences of family members to identify genes involved in addiction. First, they divide the family into two groups: affected and unaffected. Next, the researchers look for segments of chromosomes that are more common in affected people compared to unaffected. They narrow the segments down to specific genes to study further. Because people have complex and varied lives, in-depth studies are often done using animals in a controlled lab setting.
Many Genes and Pathways Influence Addiction
It is unlikely that scientists will find just one single genetic change (variant) in a single gene that causes an individual’s addiction. It is a fair assumption that like most other diseases, substance use disorder is a rather complex trait and is  influenced by variations in multiple genes, that lead to changes in very many physiological pathways, by factors from the environment, and by many other known or unknown confounding factors.
influenced by variations in multiple genes, that lead to changes in very many physiological pathways, by factors from the environment, and by many other known or unknown confounding factors.
Every person inherits a unique combination of gene variations. People with substance use disorder can have different underlying genetic causes. And people who share certain high-risk gene variations may or may not develop the trait. While finding the precise genetic cause is tricky, multiple lines of research do show that genes influence substance use. From careful studies, scientists estimate a person’s genetic outfit accounts for about 40-60 percent of the risk to actually develop an addiction; however, genetic variants may leave some individuals protected.
Discovering Addiction Genes
Studying mice has led to the discovery of many addiction-related genes, plus a deeper understanding of how these genes function in humans. To learn more about how animal models, like mice and fruit flies, have taught us so much about addiction, visit Animal Models for Addiction Research.
 Thus, like humans, mice and other animals have a reward pathway. This reward pathway functions in mice much like in humans, and many of the genes that underlie it are similar in mice and humans too. Thus, sometimes a potential addiction-related gene is discovered in people. Then animal models are used to study the functioning of the gene in depth. Other genes are discovered first in an animal model and confirmed later in people.
Thus, like humans, mice and other animals have a reward pathway. This reward pathway functions in mice much like in humans, and many of the genes that underlie it are similar in mice and humans too. Thus, sometimes a potential addiction-related gene is discovered in people. Then animal models are used to study the functioning of the gene in depth. Other genes are discovered first in an animal model and confirmed later in people.
Using these combined approaches, a fair number of genes have been detected and characterised in their functioning as addiction-related genes. Here are just a few examples of genes that influence addiction risk:
- A protective allelic variant of the alcohol dehydrogenase 2 gene (i.e., ALDH2*2) codes for a protein that can’t break down alcohol like it normally would. People with ALDH2*2 experience nausea, facial flushing, headache, and rapid heartbeat when they drink.
- Mice that make more protein from the gene Mpdz experience less severe withdrawal symptoms from alcohol and sedative-hypnotic drugs like barbiturates.
- The A1 form (allele variant) of the dopamine receptor gene DRD2 is more common in people addicted to alcohol, cocaine, and opioids. The variation likely affects how drugs influence the reward pathway.
- Mice with certain variations in the Per1 and Per2 genes drink much more alcohol than normal – especially under stress. People, especially teenagers, with specific Per1 and Per2 variations also appear more likely to follow this pattern.
- Fruit flies without the gene moody are more sensitive to cocaine. moody codes for a protein that’s needed for a healthy blood-brain barrier.
- The gene PSD-95 codes for a protein that is involved in learning and memory. Mice classified as “super-sensitive” to cocaine make about half as much of the protein compared to normal mice.
- Variations in the mu opioid receptor gene (OPRM1) change the amount of protein made. Certain variations are more common in people with opioid use disorder. Others increase the risk for alcohol dependence
- People with two copies of a certain form of the gene CHRNA5 are twice as likely to become nicotine-dependent, compared to people with two copies of a different allele. CHRNA5 codes for a protein that helps cells sense nicotine.
- In rats, missing the mGluR2 receptor adds both risk and protection. The rats get fewer rewarding effects from cocaine. If they have to work to get the drug, they tend not to bother. But if cocaine is easily available, they consume a lot of it to feel the effects.
From Genes to Treatment
Finding the genes involved in addiction is a good first step in finding therapeutic solutions. Understanding how genes cause biological differences can lead to improved treatments for substance use disorder. Each new addiction-related gene discovered is a potential “drug target”. Researchers can focus on the gene product (protein) and develop a drug to modify its activity. The goal is to correct signals or pathways and restore proper brain function.
Gene therapies are also being developed to treat addiction. One gene therapy being tested in mice generates antibodies that trap methamphetamine, preventing it from reaching the brain. In another, mice transplanted with genetically modified skin cells make an enzyme that degrades cocaine.
As we understand more about how medication effects vary from person to person, genetic tests may inform treatment. Long-term, they may be used to predict which treatments are likely to be most effective based on an individual’s genetic profile in an approach of Precision Medicine.
See here a sequence on the theme:
Disclaimer: The images and/or videos (if any) on this blog may be protected by copyright. All rights remain with the owner of these rights.


Leave a Reply
You must be logged in to post a comment.
Optional: Social Subscribe/Login